Spinal fusion is the process of joining two or more vertebrae together, immobilizing them to create a single continuous bone. It is used to treat broken vertebra, a spinal deformity, spinal weakness, spinal instability, or chronic low back pain.
Surgeons use a bone graft (extra bone tissue) — either from the patient (autograft) or a donor (allograft) — along with the body's natural bone growth processes to fuse the vertebrae. Surgeons often use implanted plates, screws, or rods to hold the vertebrae and graft to promote healing. Once this bone graft heals, the vertebrae are permanently fused.
Surgeons sometimes perform this procedure using an "open" technique, creating an incision that provides a direct line of site to the vertebra, which simplifies the process of inserting the bone graft and implants. However, this may result in damage to surrounding healthy tissue, large scars, and postoperative pain.
As an alternative, minimally-invasive surgery (MIS) uses smaller incisions and usually results in less postoperative pain and faster recovery. It does, however, require X-rays (fluoroscopy) to compensate for the surgeons lack of a direct line of site.
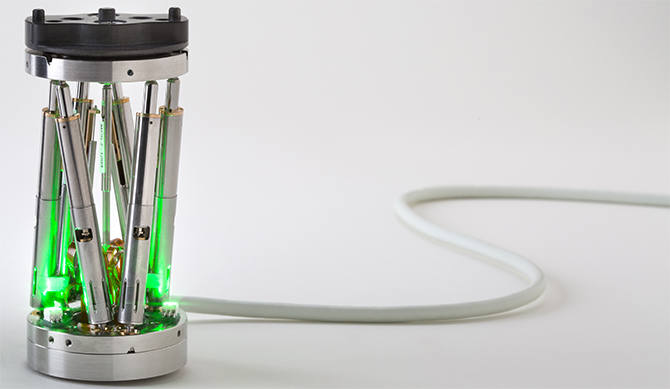
The Renaissance system guides the surgeon’s tools and implants in both open and minimally-invasive surgery (MIS), to ensure greater accuracy when compared to freehand conventional spine surgery. This can result in fewer complications, less postoperative pain, and a faster recovery. In addition, with the Mazor Robotics Renaissance Guidance System, the surgeon may require less fluoroscopy during surgery.